Tuberculosis (TB) is an infectious disease primarily caused by infection with Mycobacterium tuberculosis (Mtb). Mtb is transmitted through aerosol droplets released when a patient with pulmonary TB coughs. TB pathogenesis begins when the inhaled bacteria arrive at the alveolar region of the lungs. There resident alveolar macrophages, serving as the primary defence against pathogens, ingest the bacteria through phagocytosis and most are then eliminated at this stage. Bacteria that manages to survive this process will then multiply and result in killing of the macrophages. This eventually leads to lung damage, which is characteristic of active TB disease, moreover the infection may also disseminate to other organs in the body.
Why is TB still a global health problem?
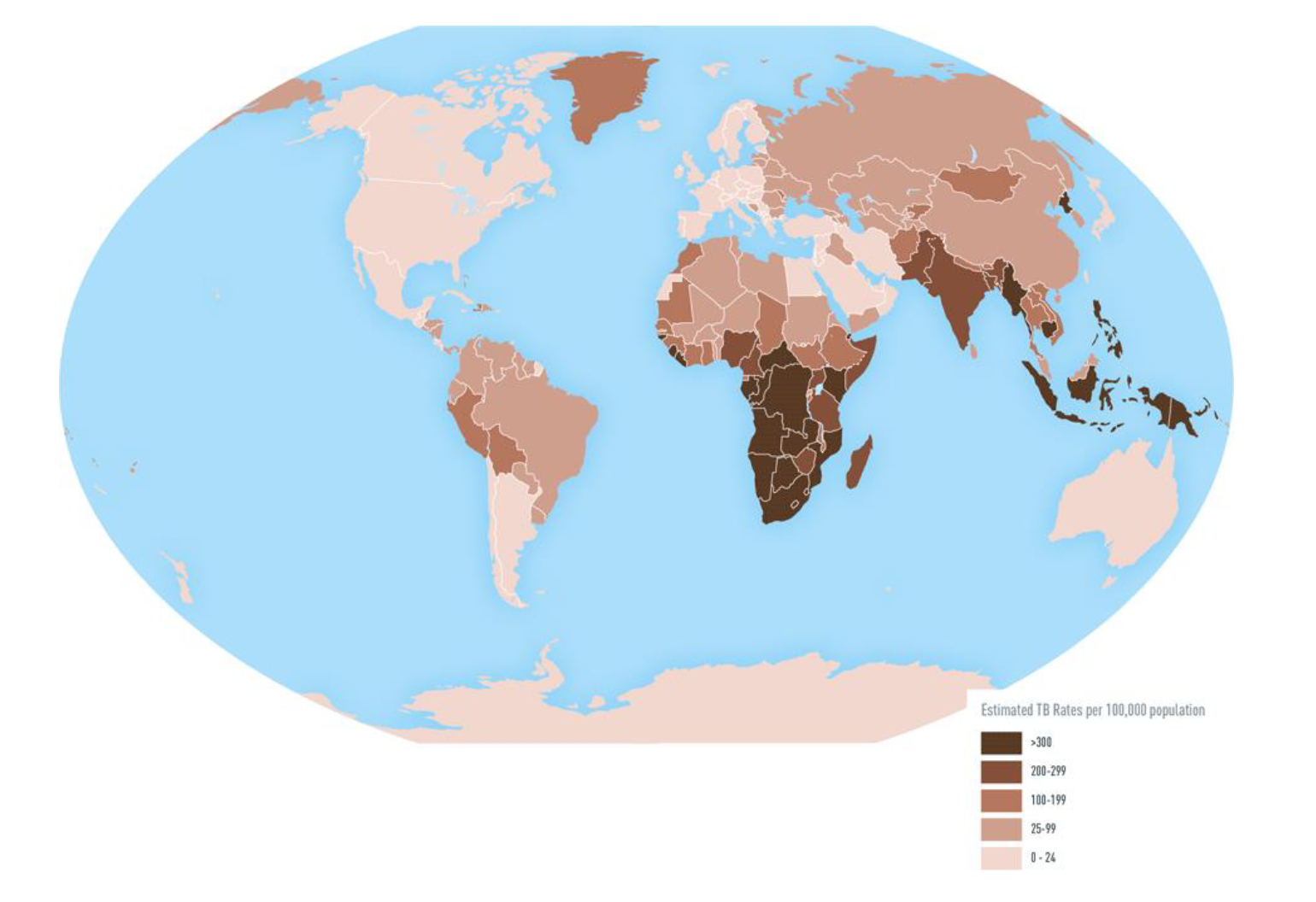
TB has existed for millennia and is one of the top ten causes of deaths worldwide. Globally, 10.4 million new TB cases and 1.7 million TB-related deaths are estimated to occur each year (see Map above). TB occurs throughout the world, but the incidence varies across each country affected. Despite the fact that most people who have active TB can be cured if treatment is administered adequately, the disease remains the leading cause of death ranking above HIV-AIDS in the past 5 years. The current tools for prevention and diagnosis have fallen short in meeting the demands required in endemic countries to reduce this on-going pandemic. The efficacy of the only licensed vaccine Bacillus Calmette-Guérin (BCG) to prevent TB is not optimal and has demonstrated different immune protection amongst individuals infected with pulmonary TB.
Why the long treatment duration?
The protracted nature of the TB treatment regimen is due to the slow response of bacterial populations to standard TB antibiotics (isoniazid, rifampicin, pyrazinamide and ethambutol), a phenomenon that is possibly attributable to persistent, and drug tolerant bacteria that resist treatment. Evidence for these types of bacterial populations has been presented in the scientific literature and in this context, the prevalence of Differentially Culturable Tubercle Bacteria (DCTB) is central. DCTB have been shown to display drug tolerance. Mtb has the ability to adopt a non-replicating state under stressful conditions within macrophages in the lungs. When these bacteria are isolated from sputum of TB-infected patients, they are unable to replicate when plated on solid media but can emerge in liquid media in the laboratory. After two months of drug treatment for pulmonary TB caused by drug susceptible bacteria, 90-95% of patients will have negative sputum or culture and show clinical improvement.
Understanding the pathogenesis of TB in efforts to combat this pandemic
An effort to identify biomarkers to predict adequate response to treatment, and biomarkers to indicate risk of developing active TB disease is of paramount importance. Innate immunity and adaptive immunity act against mycobacteria during infection. The host is initially protected from Mtb infection through adequate innate immunity, while an inadequate innate immune response results in progression of Mtb infection. The adaptive immunity then limits the growth of Mtb resulting in latent TB infection. Th1 immunity provides an important role in TB protection by inducing pro-inflammatory cytokines, which are involved in eradicating Mtb. Anti-inflammatory cytokines are the immune-regulatory molecules that inhibit the induction of pro-inflammatory cytokines, as well as opposing their biological effects. Unregulated expression of anti-inflammatory cytokines may also compromise protection provided by the pro-inflammatory cytokines.
What we found?
A previous study in our lab was done longitudinally to assess the response of DCTB to standard drug treatment. This study identified individuals who either have a rapid decline in DCTB or those with slow rates of DCTB decline. The current study used stored blood plasma samples from these individuals to assess the cytokine response to DCTB.Some pro-inflammatory cytokines were significantly elevated in the individuals who rapidly cleared DCTB compared to those who slowly cleared DCTB, during the early days of treatment while the anti-inflammatory cytokine was significantly higher in those who slowly responded to treatment. We hypothesize that pro-inflammatory cytokines promote up regulation of adaptive immune response facilitating the clearance of the bacterial infection while in contrast anti-inflammatory inhibit these pro inflammatory cytokines, support survival of the bacterium. Dichotomy in the Th1 and Th2 responses could be used to monitor the effectiveness of TB treatment thereby also identifying individuals who have a higher risk of disease relapse. Unique cytokine signatures could help elucidate immune responses that are protective against Mtb.


 Written by: Ms
Written by: Ms