Evidence Based Healthcare
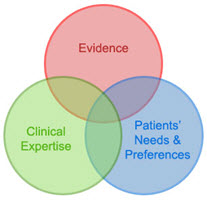 When offering health care it is important to make sure that the care being provided works. Evidence-based health care (EBHC) is “the conscientious, explicit and judicious use of the current best evidence in making decisions about the care of individual patients”[1]. It is a decision making process that takes into consideration contextual factors and combines the health worker’s expertise acquired through clinical practice and experience, current best evidence obtained from clinically relevant research, and patient values.
When offering health care it is important to make sure that the care being provided works. Evidence-based health care (EBHC) is “the conscientious, explicit and judicious use of the current best evidence in making decisions about the care of individual patients”[1]. It is a decision making process that takes into consideration contextual factors and combines the health worker’s expertise acquired through clinical practice and experience, current best evidence obtained from clinically relevant research, and patient values.
It is recommended that EBHC becomes an integral part of learning in the curriculum of all health care professionals, since learning the fundamentals of research and the basic knowledge and skills of EBHC are essential for successful implementation of EBHC and subsequent improvement in quality of healthcare[2]. This is also highlighted in the recent Lancet report on the health professional for the 21st century, which proposes a shift from memorization of facts to “critical reasoning that can guide the capacity to search, analyse, assess and synthesise information for decision-making”[3].
The EBHC subproject of SURMEPI aims to enhance teaching of EBHC at under- and postgraduate, as well as health care professionals working in the field. The specific activities fall under the following goals and objectives of the overarching project:
Goals
- To increase the quality of health care provision, particularly by medical doctors, in rural and under served areas.
- Objective: enhance the teaching and learning experience (including the curriculum) for undergraduate medical students to increase exposure to critical elements of primary health and related issues, in order to prepare them for a career in rural medicine.
- To increase in the retention of health care workers over time in areas where they are most needed.
- Objective: to enhance the capacity and quality of health care workers, specifically medical practitioners in rural and under served areas with a view to increase retention.
- To establish SURMEPI as a hub for regionally relevant research in support of MEPI goals and in collaboration with MEPI partners.
- Objective: to establish a culture of conducting and using regionally relevant research among students and, where relevant, medical practitioners in rural/under served areas.
Key outputs:
- Publications:
- Young T, Rohwer A, Volmink J, Clarke M (2014) What Are the Effects of Teaching Evidence-Based Health Care (EBHC)? Overview of Systematic Reviews. PLoS ONE 9(1): e86706. doi:10.1371/journal.pone.0086706
- Rohwer A, Rehfuess E, Young T. E-learning of Evidence-Based Health Care to Increase EBHC Competencies in Healthcare Professionals. 2014 (http://www.campbellcollaboration.org/lib/project/224/)
- Rohwer A, Young T, van Schalkwyk S. Effective or just practical? An evaluation of an online postgraduate module on evidence-based medicine (EBM). BMC Medical Education 2013,13:77 (http://www.biomedcentral.com/1472-6920/13/77)
- Poster presentations:
- Rohwer A, Rehfuess E, Young T. E-learning of evidence-based health care (EBHC) to increase EBHC competencies in healthcare professionals: A systematic review
- Rohwer A,Young T. Recent medical graduate’s opinion on Evidence-based Health Care (EBHC) in Stellenbosch University’s medical curriculum
- Rohwer A, Schoonees A, Engel M, Young T. Enhancing evidence-based health care (EBHC) knowledge and skills of medical student interns at Stellenbosch University’s Rural Clinical School in Worcester
- Rohwer A, Young T, van Schalkwyk S Teaching evidence-based medicine (EBM) to specialists – Evaluation of a web-based module on EBM for Family Medicine specialists in training at Stellenbosch University.
- Rohwer A, Young T. Document review of the undergraduate medical curriculum at Stellenbosch University to inform enhancement of evidence-based health care (EBHC) teaching
Useful resources: